Industry Best Practices for Measuring and Reducing Patient No-Shows
Introduction
Patient no-shows permeate medical practices, across specialties, locations, and practice models. While no-shows consistently cause problems for practices, not all practices track their no-show rate or realize the impact that even a couple daily no-shows can have on both their processes and their revenue.
There are many reasons that patients fail to make their appointments and there are demographic similarities across patients who no-show more consistently than others. Practice managers work hard to reduce no-shows using a variety of strategies, but often those strategies involve manual processes or difficult-to-enforce policies, resulting in a low impact.
With the rise of EHR’s, Meaningful Use, and innovation in healthcare, the industry has developed some best practices to offer practice managers that eliminate manual work and have been shown to decrease no-show rates by over 50%.
This definitive guide explores the underlying causes of no-show behavior, outlines best practices, and shares how they work to reduce the manual workload of practice staff, serve patients better, and ultimately reduce patient no-shows.
Practice Management Has Many Challenges, No-Shows Doesn’t Need to Be One
Practice Manager. Clinical Manager. Patient Access Manager.
Your background may be clinical, administrative, or financial—if you’re running the day-to-day operations of one or more medical practices, we know you’re hustling to keep efficiency and productivity at its peak. And it’s a tough gig—balancing staff and physician needs, billing, insurance, patients, and scheduling while trying to tackle the challenges of manual processes, silo-ed systems, and the general daily hiccups associated with providing care to patients. If you’ve been asking yourself the best way to reduce patient no-shows and engage patients in their own care, we can help.
What is a patient no-show? A patient no-show refers to a missed patient appointment wherein the patient was scheduled, did not appear for the appointments, and made no prior contact with the clinic staff.
Patient No-Shows: Who does it, why, and what you can do to change it
You’ve experienced it: idle physicians, waiting patients, and last minute vacancies—no-shows put patients behind in their care and negatively impact downstream processes.
- Patient no-shows cost the healthcare industry $150 billion annually
- For a primary care physician, each missed appointment equals roughly $150-$200 in lost revenue. For surgeons, this is closer to $500.
- Patients who fail to show up for their appointments often require more expensive emergency care later on. These higher costs get factored into healthcare costs for everyone else
“For specialty practices that often have long wait lists, a patient no-show means that a wait-list patient has been waiting too long to see a physician and more importantly, could have had a spot on the schedule, but didn’t have the opportunity. Timing and access is everything for our patients.”
Sadaf Tehrani
Director Patient Access and Scheduling, Children’s Hospital Colorado
Why It’s Important to Track Your Patient No-Show Rate
Medical practices should track their patient no-show rates because without accurate numbers to reflect baseline data and progress, it’s impossible to quantify the results of any efforts to reduce patient no-shows. Have reliable no-show data is also important because it represents lost revenue for the practice or medical group. Recapturing that revenue can mean financial health for a medical practice and can be used to add staff, invest in new or additional resources, upgrade technology, and improve employee salaries and benefits. For example: if a single-provider practice averages two no-shows daily, the missed revenue (approximately $104,000 annually) could mean the ability to add 1-2 full-time staff members.
How you define a “no-show” is just as important as establishing a way to track it. In our experience, we’ve seen two common mistakes that can unintentionally result in misleading data:
1. Including cancellations and appointment changes into their no-show rates
2. Marking a no-show as “canceled”
Practices in both of these scenarios struggle because they are operating with bad numbers.
Defining a Patient No-Show for Measurement
For benchmarking, a no-show is defined as a patient who never arrived for a scheduled appointment and gave no prior notice.
How to Calculate Your No-Show Rate
Take the total number of patients that did not show up for their appointment and divide by the total number of scheduled appointments (if you remove appointments that no-show, be sure to add them back to calculate). No-Show Rate = No-Shows / Scheduled Appointments* *remove walk-in appointments

Why Patients Miss Appointments
Anyone can be guilty of missing an appointment, though patients who are most likely to miss their appointments share some common demographics, including:
- single/unmarried
- are 34 years of age or younger
- are on Medicaid or have no coverage at all
- have chronic conditions
- are older and are recently widowed or divorced
- live 60 miles or more from the clinic location
Demographics aside, patients miss appointments for several reasons. Without understanding what contributes to missed patient appointments, practices and healthcare organizations can unknowingly contribute to the problem.
These are the top five reasons patients miss their appointments.
Forgetfulness
Forgetfulness is the #1 reason patients report for not showing up for their appointments; to compound this problem, 24% of patients in one survey said they tried to cancel their appointment but couldn’t.
Time
Patients will often accept an appointment that isn’t convenient because it appears to be their only option but will later no-show because their schedules truly couldn’t accommodate the appointment dates and/or times from the beginning.
Cost
While the rate of insured patients has dropped in recent years, copays, deductibles, and out-of-pocket expenses have risen dramatically. Patients fearing they won’t be able to afford their portions of their medical bills will sometimes avoid appointments altogether because they are too embarrassed to discuss the financial burden.
Fear
Patients have anxiety about visiting their providers—these anxieties and fears are easily overlooked by clinical staff who handle medical interactions on a daily basis. Procedures, bad news, and disapproval from a physician can all be contributing fears that cause patients to avoid their appointments.
Demographic barriers
Language and age are two examples of demographic barriers that can result in a patient no-show. Consider the elderly patient who no longer drives, a failure or unforeseen change to their transportation plan may leave them without a way to get to their appointment and without the time to notify the clinic.
How to Deal with Patient No-Shows
Strategies That Don’t Work for Reducing Patient No-Shows
We can impact nearly every reason that patients no-show with patient-centered communication. Of course, for every great strategy that delivers results, there’s one that didn’t pan out and we’ve seen it all. First generation solutions to patient no-shows were well-intentioned but failed to deliver results, here a few of the most common.
No-Show Appointment Policy: Charging Patients for Missed Appointments
Roughly 25% of physician practices charge some kind of no-show fee. Practices use this strategy in hopes that charging a fee will force a patient to connect value to a physician’s time, will recover a small portion of lost reimbursement, and will alter patient behavior even if a practice never intends to collect the fee. Charging a fee for missed appointments yields only small improvements in patient no-show rates, partly because many practices fail to inform patients they have no-show policies in place. In a recent survey, MGMA found that 41.6% of patients who missed an appointment, said they were unaware of their doctor’s no-show policy. This strategy also creates additional work for staff and fails to address many of the underlying reasons that patients miss their appointments. Finally, Medicaid doesn’t allow medical practices to charge patients for missed appointments in some states yet Medicaid patients are one of the more likely patient types to no-show, rendering this type of no-show strategy ineffective for a large percentage of a practice’s patients.
Voice-Only Appointment Reminders
Voice-only appointment reminders fall short because patients rarely answer their phones or respond to voicemail. Robocalls and phone scams have dissolved consumer trust in phone calls from numbers that they don’t recognize and most prefer to communicate via text. The success of voice-only reminders hinge on patients answering their phones because if the call is missed, the patient has no opportunity to confirm, cancel, or reschedule the appointment—something that is pivotal to a successful no-show reduction strategy.
Double Booking Appointments
Double booking appointments banks on the probability that a patient won’t show up for their appointment. When patients do show up as scheduled, the results are long wait times, frustrated patients, and minimal time with a provider— all of which put the hard-earned reputation of the practice in jeopardy and require double the work for staff. While double booking may serve as a short-term solution, in the end it requires more work for the same amount of revenue.

Best Practices & Tangible Solutions
As you move towards solving your patient no-show problem, keep it simple. Your goal should be to engage your patients in a way that is intuitive and reduces work for your staff—here are some best practices that have the proven ability to revolutionize your practice for both your patients and your staff.
Automated Appointment Reminders
Automation is key to implementing a solution that is sustainable over time and can grow with your practice. Start by making a list of all the manual activities your staff is doing to engage patients and reduce no-shows. We are willing to bet that most, if not all, of those manual processes could be automated—freeing up the valuable time of your staff. Automating your reminders also reduces the risk of errors and gaps in communication. If reminders don’t require the time and attention of a human, they won’t get reprioritized when the clinic has a rush or is short-handed for a day.
“We used to have nurses call the high-risk families every couple of days prior to their appointment to remind them, which isn’t the best use of a nurse’s time.”
Katie Schuman
Associate Clinical Manager, Children’s Hospital Colorado
Use Intuitive Tech
At Relatient, we talk a lot about being patient-centered, it’s the force behind everything we do. Our products and best practices are designed to be invisible because we want patients to engage with their physicians without even thinking about it. We’ve learned a couple things about patient behavior and know that adoption happens when:
- We use existing technology
- The solution doesn’t require a username or password
- The solution doesn’t require the user to download an app
- A relevant message is delivered at the right time
We utilize tech that’s already in hands of patients— with text (sms) messaging. SMS is on every phone, it’s been around longer than the iPhone, and it’s easy enough for a child to do. Check out these statistics:
- Adults under 45 send and receive 85+ texts every day, on average, while adults 45-54 send and receive 33 texts a day, and adults 55+ send and receive 16 texts a day.
- People prefer text most for scheduling or changing appointments. In fact, 78% of people wish they could have a text conversation with a business, and 64% of consumers report they are likely to think positively of companies that communicate via text.
- Text messages produce a 209% higher response rate than phone calls, and confirmation via text is 295% more successful than phone calls.
- Texting is the highest rated contact method for customer satisfaction compared to all other communication channels (Text – 90; Phone – 77; Facebook – 66).
This strategy is so effective, we’ve seen practices reduce their patient no-show rates by 40%-50% within weeks of implementation, giving them the ability to add appointments back to their schedules every week. This sends productivity through the roof and dramatically increases revenue by getting patients that are already scheduled in the door and moving waitlisted patients to an open slot in the schedule.
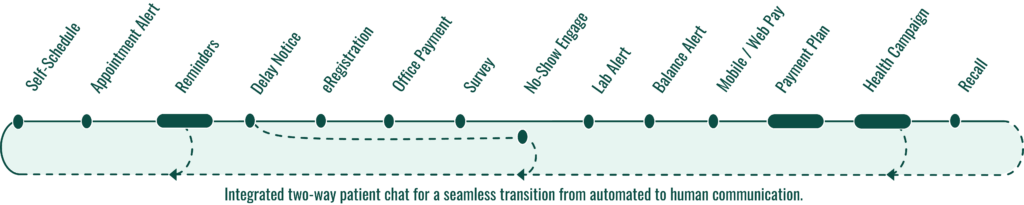
Leverage Multiple Communication Methods
A good strategy is comprehensive, it doesn’t assume all patients are equal. While evidence shows that text messages have the highest response rate and are capable of reaching the greatest percentage of patients, email and voice are also important components of a patient engagement strategy. The key is that every message utilizes a modality that can be pushed to a mobile device and leverages a strategic timeline to trigger the right patient behavior. If a message is sent to a patient too far in advance of an appointment, there’s a higher chance the patient will disregard. If no communication is sent until the day of an appointment, it may be too late for the patient to work it into their schedule. Using a combination of communication methods triggered at specific times prior to the appointment keeps the communication top-of-mind for the patient and increases the likelihood that they will confirm and attend as-scheduled or communicate any conflicts and free up the appointment for a waitlisted patient.
Utilize Bi-Directional Communication
Bi-directional communication refers to the ability for your automated appointment reminders to send data back and forth to your scheduling software, often referred to as your practice management system. Reducing the manual burden on staff and creating new efficiencies requires an integration to your EHR or practice management system so the data is readily available and staff can act on it accordingly. Case in point—Oklahoma Heart Hospital left a first-generation reminder system whose integration didn’t deliver as-promised and made their data difficult to access. When they switched appointment reminders to Relatient, the integration with Cerner made it easy for schedulers and managers to see which patients needed rescheduled and which had not confirmed their appointments yet. The ability to access patient data and respond proactively is saving this large cardiovascular specialty group nearly $1 million annually.
Finding the Right Vendor
You’ll need some help to automate your processes and put some of these practices in place. Choosing a partner can be overwhelming, but evaluating your options based on the things that will improve your patient satisfaction, provide new efficiencies, and reduce wasted time and effort will quickly narrow your list.
We’ve spent years asking our customers what’s important to them in a long-term partner and how they chose Relatient. Below is a list of questions our customers have asked us and we’ve learned these are central to the success and ROI for medical practices, individual providers, and healthcare systems alike.
- Functionality: Can the system accommodate multiple sites, multiple families on one contact number, and multiple modes of communication?
- Is it bi-directional? What happens to patient response data and how will you capture it?
- How is the product priced? Is there a cap on the volume of messages sent?
- What kind of service will you get after go-live? Will you have the option to talk to a human during the most critical hours of operation?
- Can patients confirm, cancel, or request to reschedule from the appointment reminder?
- How complicated is the go-live process and what kind of support will you have along the way?
- Will your patients need to access a portal, download an app, or use a username and password to engage through this solution?
- How will your vendor partner with you to keep you compliant with TCPA regulations?
- How well does this partner understand your greatest challenges and priorities? Are they healthcare experts and what additional expertise do they bring to the table?
“We didn’t want a report workaround; we wanted a seamless integration. Not an externall, stand-alone, silo-ed system.”
Jason W. Miller
CEO, Reiter, Hill, Johnson & Nevin
Finding the right partner to help you identify existing gaps, match you with the right solutions, and provide long-term support and training will do more than just lower patient no-shows. This kind of collaboration helps equip medical practice managers with the tools and solutions that deliver efficiency, patient satisfaction, and a streamlined patient experience that isn’t possible with manual processes or silo-ed systems. Reiter, Hill, Johnson & Nevin, a long-time Relatient customer and multi-provider women’s health practice, found that implementing appointment reminders eliminated 200-300 manual outbound calls per day, freeing their staff to focus on incoming calls from patients. They were also able to completely eliminate all postcards and the staff costs associated with sending out reminder postcards for their practice.
Conclusion
Few practices are immune to the impact of no-shows and practices who don’t perceive patient no-shows to be a problem are missing an opportunity to increase revenue and fill open appointments in their schedules.
With the many demands placed on practice managers, resources are thin yet many practices still rely on manual processes like phone calls and post-cards to remind patients of their appointments or are using outdated solutions that lack the proven best practices for reducing patient no-shows. Automation and patient-centered practices offer medical practices solutions to their no-show problems that operate in the background and require minimal work from practice staff. This frees staff to focus on patient care, strong documentation, and follow-up.
There are many vendors in the marketplace who offer some form of patient appointment reminders, few offer the functionality and support that make automation an efficient solution for practices.
Bottom line: patient no-shows are a hassle, but they’ve got nothing on you. Go get ’em.